Comprehensive Guide to Modern Breast Augmentation Procedures: Understanding Your Options
Breast augmentation represents one of the most frequently performed cosmetic surgical procedures worldwide. The procedure fundamentally involves enhancing the size, shape, and overall aesthetic appearance of the breasts through surgical intervention. When you consider breast augmentation, you’re looking at a procedure that modifies the anatomical structure of the chest by introducing implantable devices or autologous tissue to achieve volume enhancement and contour refinement.
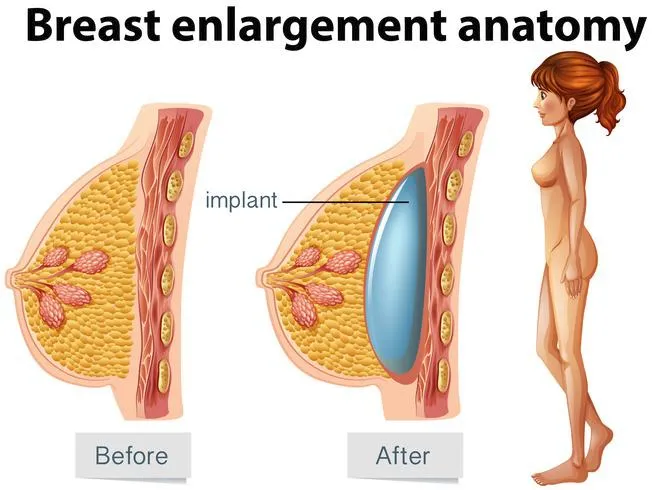
The mammary gland itself is composed of glandular tissue, supportive fibrous tissue, and adipose (fat) tissue, all contained within a cutaneous envelope. The procedure targets this anatomy by creating a surgical pocket, typically in one of several anatomical planes: subglandular (between the breast tissue and pectoral muscle), submuscular (beneath the pectoral muscle), or using the dual-plane technique (a hybrid approach utilizing both planes). This surgical manipulation creates space for the introduction of an implant or transferred tissue.
The concept of breast modification has existed throughout human history, but modern medical breast augmentation emerged in the mid-20th century. The first silicone breast implant was introduced in 1962, marking the beginning of contemporary approaches to the procedure. Prior to this medical innovation, women seeking breast enhancement relied primarily on external prosthetics, padded garments, or experimental substances that often led to significant complications.
Throughout history, breast size and shape have carried cultural significance across various societies, but the concept of surgical enhancement specifically for cosmetic purposes is relatively recent. Earlier civilizations didn’t have access to the medical technology required for safe augmentation. The procedure gained substantial momentum during the latter half of the 20th century as surgical techniques improved, implant technology advanced, and societal acceptance increased.
The evolution of breast augmentation has been marked by significant advancements in both technique and materials. Early implants faced challenges including rupture, capsular contracture, and safety concerns. Modern implants utilize medical-grade silicone shells filled with either saline solution or cohesive silicone gel, dramatically improving safety profiles and aesthetic outcomes. Surgical approaches have similarly evolved, with refinements in incision placement, implant positioning, and tissue handling all contributing to enhanced results and reduced recovery time.
Today, when you pursue breast augmentation, you benefit from decades of medical advancement, with procedure options that can be customized to your specific anatomical requirements, aesthetic goals, and lifestyle considerations. The modern approach emphasizes not just enhancement, but natural-appearing results, proportional outcomes, and long-term safety considerations.
Types of Breast Augmentation
Comparison of Breast Implant Types
| Feature | Saline Implants | Silicone Gel Implants | Form-Stable (“Gummy Bear”) Implants |
|---|---|---|---|
| Composition | Silicone shell filled with sterile saltwater solution | Silicone shell filled with moderately cohesive silicone gel | Silicone shell filled with highly cohesive silicone gel that maintains shape when cut |
| Feel | Firmer, less natural feel; may have water-ripple effect | Soft, natural feel similar to breast tissue | Firmer than traditional silicone but maintains shape; slightly less natural feel |
| Incision Size | Smaller (2.5-3.5cm); inserted empty then filled | Larger (4-5cm); pre-filled | Largest (5-6cm); pre-filled and firmer consistency |
| Rupture Detection | Immediately noticeable; breast deflates as saline is absorbed by body | Silent rupture; requires MRI or ultrasound for detection | Silent rupture but gel maintains shape; requires imaging for detection |
| Rupture Concerns | No health risks; saline safely absorbed by body | Gel may remain contained in capsule but recommended removal | Highly cohesive gel remains intact and in place; minimal migration risk |
| Shape Options | Round only; loses shape when upright | Round or anatomical; moderately maintains shape | Primarily anatomical/teardrop; excellent shape retention |
| Natural Movement | Less natural movement; moves as a unit | Natural movement similar to breast tissue | Maintains shape during movement; less natural mobility |
| Rippling Risk | Higher (7-12%); especially in thin patients | Moderate (3-7%); less visible than saline | Lowest (1-3%); excellent edge concealment |
| Capsular Contracture Risk | 10-15% at 10 years | 10-12% at 10 years | 7-9% at 10 years |
| FDA Approval Age | 18+ years for cosmetic augmentation | 22+ years for cosmetic augmentation | 22+ years for cosmetic augmentation |
| Monitoring Requirements | Standard breast exams; rupture immediately visible | MRI or ultrasound recommended at 5-6 years, then every 2-3 years | MRI or ultrasound recommended at 5-6 years, then every 2-3 years |
| Incision Approaches | All approaches viable (inframammary, periareolar, transaxillary, transumbilical) | Limited to inframammary, periareolar, and transaxillary (with limitations) | Primarily inframammary; periareolar possible with large areola |
| Breast Shape Result | Rounder upper pole; fuller appearance | Natural slope in upper pole; versatile shape options | Most natural contour; defined lower pole with tapered upper pole |
| Rotation Concern | No concern (round shape) | Only with anatomical shapes (minimal concern with round) | Significant concern (1-3%); requires precise pocket creation |
| Cost Comparison | Lowest cost option | $1,000-1,500 more than saline | $1,500-2,500 more than saline |
| Ideal Candidates | Patients with adequate breast tissue; those seeking cost-effective option; younger patients (18-22) | Patients desiring natural feel and appearance; those with minimal existing breast tissue | Patients seeking anatomical shape; those with tissue laxity or tuberous breasts; athletic patients |
| Longevity | 10-15 years average; higher annual rupture rate (1-2%) | 10-20 years average; lower rupture rate (0.5-1% annually) | 10-20+ years; potentially longer-lasting due to shell integrity and gel stability |
Saline Implants

Saline breast augmentation is a surgical procedure that enhances breast size and shape using implants filled with sterile saltwater. The procedure involves making small incisions, usually near the breast crease, through which empty saline implants are inserted. Once in place, the implants are filled with a sterile saltwater solution, allowing for smaller incisions compared to pre-filled implants.
Saline breast implants consist of a durable silicone outer shell filled with a sterile saltwater solution. When considering breast augmentation, it’s essential to know that saline implants offer consistent shape, firmness, and feel. One significant advantage is that these implants are inserted empty and then filled after placement, enabling smaller incisions compared to pre-filled silicone implants.
Saline implants have a robust safety profile regarding leakage. If an implant rupture occurs, the saline solution is harmlessly absorbed by the body and naturally expelled through regular physiological processes. Detection of a rupture is immediate and apparent, as the affected breast will visibly deflate. This quick detection eliminates the need for routine imaging, unlike silicone implants, where ruptures might initially go unnoticed.
Historically, saline implants were the exclusive option available during the FDA-imposed restrictions on silicone implants between 1992 and 2006, largely due to their reliable safety record.
However, saline implants may produce less natural-looking results, especially for individuals with limited breast tissue. Implant edges may become visible or palpable, particularly around the upper breast area or the breast’s outer edges. Rippling or wrinkling may also occur if the breast tissue covering the implant is thin, though experienced surgeons can significantly reduce these effects through precise implant placement techniques.
From a maintenance perspective, saline implants generally require less surveillance than silicone implants. Routine MRI scans to check for silent ruptures are unnecessary, simplifying long-term care. Saline implants are FDA-approved for breast augmentation in individuals 18 years or older, providing a suitable alternative for younger patients ineligible for silicone implants.
The benefits of saline breast augmentation include smaller incisions, natural absorption of the saline solution if an implant ruptures, and easy detection of rupture due to immediate deflation. If an implant ruptures, the body can naturally absorb the saline solution, making it a safer option.
While saline implants offer notable safety and maintenance advantages, they may feel firmer and slightly less natural compared to silicone implants or natural breast tissue. Additionally, saline implants tend to weigh more, which over time might contribute to increased tissue stretching. Understanding these characteristics will help you make an informed decision tailored to your personal and aesthetic goals.
- Read This Post Saline Implants – What You Need To Know? – To Get Complete Overview
Silicon Gel Implants
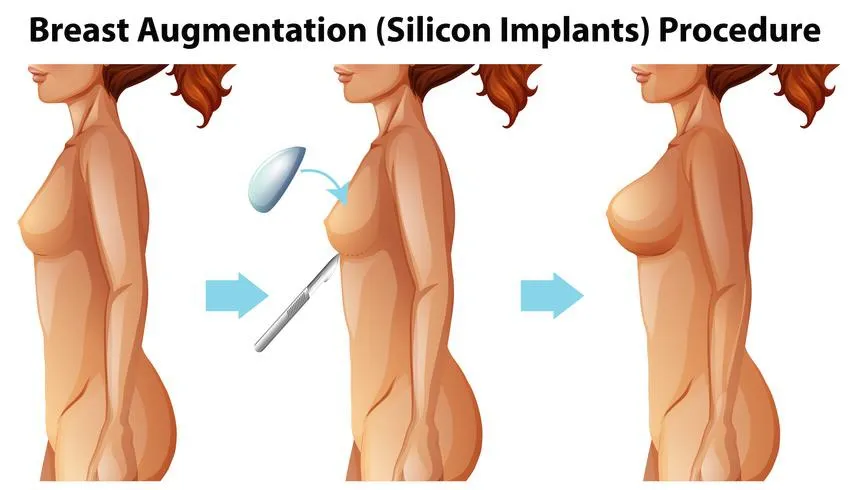
Silicone gel breast augmentation is a surgical procedure that involves the placement of silicone gel-filled implants to enhance the size and shape of the breasts. The silicone gel implant consists of a durable silicone outer shell filled with a cohesive gel that mimics the feel and consistency of natural breast tissue. This procedure is typically performed under general anesthesia and takes about one to two hours. The surgeon makes an incision, usually beneath the breast, around the areola, or in the armpit, to insert the silicone implants either above or below the chest muscle, depending on the patient’s anatomy and goals.
Silicone gel implants consist of a silicone outer shell filled with a cohesive silicone polymer gel. These implants come pre-filled in various sizes, shapes, and profiles, offering a range of options for breast augmentation. The silicone gel inside these implants has evolved over time, with modern formulations designed to maintain shape and consistency, even if the outer shell is compromised. The cohesive gel is engineered to resemble natural breast tissue, with its density and viscosity providing a more natural feel compared to saline implants.
One key advantage of silicone implants is their ability to provide a natural look and movement, making them particularly suitable for patients with minimal breast tissue. The gel within these implants mimics the feel of natural breast tissue, leading to a more aesthetically pleasing and realistic outcome. Silicone implants are also available in a variety of profiles and shapes, allowing for customization based on the patient’s body and desired outcome.
However, it’s important to be aware of some unique considerations with silicone implants. Unlike saline implants, a rupture in a silicone implant doesn’t lead to immediate deflation or noticeable asymmetry. This phenomenon, known as a “silent rupture,” may go undetected without imaging studies such as MRI or ultrasound. Because of this, regular monitoring is recommended by the FDA, typically through imaging every few years, to ensure the integrity of the implants.
- Read This Post: Silicone Gel Implants For Complete Guide
Form-stable (“gummy bear”) Implants

Form-stable implants, often referred to as “gummy bear” implants, are a cutting-edge advancement in silicone implant technology. These implants are filled with a highly cohesive silicone gel that is designed to maintain its shape, even if the implant is cut. The key feature of form-stable implants is their molecular structure, where the silicone is cross-linked to a higher degree compared to traditional implants. This results in a more solid and stable material that resists gel migration, even if the outer shell is compromised.
The implants are typically shaped in an anatomical or teardrop form, designed to mimic the natural contours of the breast. Unlike round implants, which can create an overly full appearance, the teardrop shape provides a more subtle and natural slope, particularly in the upper part of the breast. This makes them an ideal choice for patients seeking a more realistic, natural result.
One of the key benefits of form-stable implants is their ability to retain their shape and provide a natural appearance. They are available in various shapes, including anatomical or teardrop shapes, which mimic the natural slope of the breast. This makes them an ideal choice for patients seeking a more natural look and feel. During the procedure, the surgeon will select an implant size and shape that is tailored to the patient’s individual anatomy and desired outcome.
The recovery process for breast augmentation with form-stable implants is relatively straightforward. Patients can expect a few days of rest and minimal discomfort, with the final results becoming visible as swelling subsides. Overall, form-stable implants are a reliable choice for patients looking to enhance their breast volume while maintaining a natural aesthetic.
When considering gummy bear implants for a patient, several factors must be taken into account, including breast tissue quality, the desired aesthetic outcome, and the patient’s anatomy. These implants require adequate tissue coverage to avoid being palpable, but their resistance to rippling makes them a favorable option for individuals with less natural breast tissue. Overall, form-stable implants offer a durable, aesthetically pleasing solution for patients looking for a long-lasting and natural-looking result.
- Read This Post: Form-stable (“gummy bear”) Implants For Complete Guide
Fat Transfer Breast Augmentation
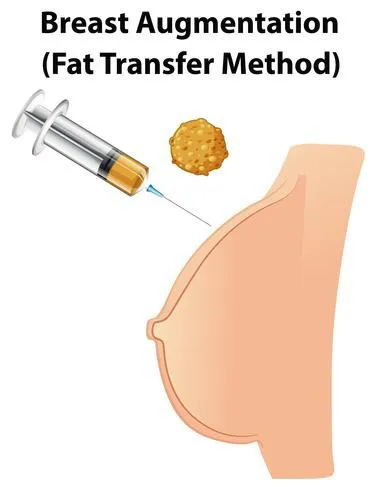
Fat transfer breast augmentation, also known as autologous fat transplantation or natural breast augmentation, involves harvesting adipose tissue from one area of your body and transferring it to your breasts to enhance their size and shape. This technique uses your own body fat as a natural filler, avoiding the need for prosthetic implants while creating subtle, natural-appearing results.
The procedure represents a fusion of liposuction techniques with specialized fat processing and injection methodologies. When considering this approach, it’s important to understand that fat transfer augmentation fundamentally differs from implant-based procedures in both technique and outcomes. As a completely autologous procedure, it utilizes only your own tissues, eliminating concerns about foreign body reactions or implant-specific complications.
When I evaluate candidates for fat transfer augmentation, I assess both potential donor sites and breast characteristics. The procedure requires sufficient donor fat for harvesting while having appropriate breast tissue for successful fat infiltration and retention. The technique has evolved significantly over the past decade, with refinements in harvesting, processing, and injection techniques substantially improving fat survival rates and predictability of outcomes.
Fat transfer breast augmentation offers a dual benefit – removing fat from areas where it’s unwanted while enhancing breast volume. This approach appeals to patients seeking modest size increases with completely natural feel and appearance. Unlike implant-based techniques, fat transfer results integrate completely with your existing breast tissue, creating seamless results without distinct edges or boundaries.
Harvesting Technique
The fat transfer procedure begins with liposuction to collect adipose tissue from appropriate donor sites on your body. When performing this harvesting phase, I carefully select areas with adequate subcutaneous fat deposits that respond well to liposuction contouring. Common donor locations include the abdomen, flanks (love handles), thighs, and lower back.
The harvesting technique substantially impacts fat cell viability and ultimately the success of the procedure. I employ specialized cannulas (thin, hollow tubes) connected to gentle suction systems designed specifically for fat transfer procedures. These systems utilize larger diameter cannulas (3-4mm) with multiple side holes and operate at lower negative pressures than traditional liposuction. This gentle approach preserves fat cell integrity during collection, maintaining cellular viability for subsequent transfer.
I perform the harvesting using tumescent technique, which involves infiltrating the donor areas with a dilute solution of lidocaine (local anesthetic) and epinephrine (to minimize bleeding) before extraction. This solution makes the fat extraction less traumatic to the cells while providing pain control during and after the procedure. The harvested fat appears as a mixture of fat, blood, and tumescent fluid that requires specialized processing before injection.
The choice of donor site influences both the quality of harvested fat and the secondary contouring benefit. Abdominal fat typically provides excellent volume and consistent quality, while thigh fat often contains slightly larger fat lobules. I select donor areas based on your individual fat distribution pattern, targeting zones with suitable fat density while considering the aesthetic improvement of removing fat from these regions.
For optimal results, I typically harvest 3-4 times the volume ultimately needed for injection, as processing removes a significant portion of non-adipose fluids and some fat cells inevitably fail to survive the transfer process. Patients with limited donor fat may not be ideal candidates for significant augmentation using this technique, as adequate source material is essential for meaningful enhancement.
Fat Processing Methods
Once harvested, the fat requires careful processing to isolate healthy adipocytes (fat cells) from unwanted components such as blood, oil, and tumescent fluid. This purification step critically impacts graft survival rates and overall procedure success.
I utilize specialized fat processing systems that employ centrifugation, filtration, or washing techniques to purify the harvested material. Centrifugation involves spinning the collected lipoaspirate at specific speeds to separate it into three distinct layers: an upper oil layer (from damaged fat cells), a middle layer of purified fat cells, and a lower layer of blood and tumescent fluid. I carefully isolate and preserve only the middle layer containing viable adipocytes.
The processing technique requires precise calibration to balance purification with cellular trauma. Excessive centrifugation speeds or aggressive handling damages delicate fat cells, reducing survival rates after transfer. Conversely, inadequate processing leaves inflammatory mediators and debris that interfere with graft integration. The processing approach significantly influences overall retention rates, with studies showing 10-30% differences in long-term survival based on handling techniques.
Some advanced procedures utilize additional biologic enhancement during processing. Platelet-rich plasma (PRP) derived from your own blood may be added to the processed fat to introduce growth factors that potentially improve vascularization and fat cell survival. Similarly, adipose-derived stem cell concentration techniques aim to enrich the graft with regenerative cells that support long-term viability. These supplementary approaches remain under investigation but show promising results in improving the predictability of volume retention.
The processed fat requires careful handling before injection, as exposure to air or excessive warming damages cells. I transfer the purified fat into specialized syringes designed for immediate use, maintaining sterile technique throughout to prevent contamination that could lead to inflammation or infection after placement.
Injection Technique
The injection phase represents the most technically demanding aspect of fat transfer breast augmentation. When performing this stage, I utilize specialized blunt-tipped cannulas specifically designed for fat grafting to the breast. These instruments allow precise, controlled placement of small amounts of fat in multiple layers and locations throughout the breast tissue.
The injection technique follows the principle of structural fat grafting, which emphasizes placing micro-droplets (1-4mm) of fat in multiple passes and layers rather than larger boluses. This creates a three-dimensional lattice of transplanted fat cells, ensuring each droplet remains in close proximity to your existing vasculature. Fat cells must establish blood supply within 48-72 hours to survive long-term, making this proximity essential. Micro-droplet technique maximizes the surface area of transferred fat exposed to surrounding tissues, optimizing nutrient diffusion and neovascularization (new blood vessel formation).
I carefully place the fat in multiple anatomical planes of the breast, including the subcutaneous space, within the breast parenchyma (actual breast tissue), and in the prepectoral space (in front of the chest muscle). This multi-level placement creates natural-appearing enhancement while maximizing the total volume that can be successfully integrated. Areas requiring special attention include the upper pole, medial breast border, and inframammary fold, where precise enhancement significantly impacts overall breast shape and profile.
Technical considerations include injection pressure and speed, which directly affect fat cell survival. I utilize low-pressure, slow injection techniques that minimize cellular trauma during placement. The specialized cannulas feature side holes rather than end openings, preventing excessive pressure at the injection site while allowing smooth distribution of the fat grafts.
The total injectable volume per session ranges from 100-300cc per breast, depending on your existing breast size, tissue elasticity, and vascularity. Attempting to transfer excessive volumes in a single procedure significantly reduces retention rates due to inadequate vascularization. Patients desiring larger augmentation often require staged procedures spaced 3-6 months apart to allow complete healing and vascularization between sessions.
Volume Retention
Fat transfer breast augmentation produces substantial but not complete volume retention after the procedure. When discussing expectations with patients, I emphasize that some degree of volume loss inevitably occurs as a normal part of the healing process. Understanding these retention patterns helps establish realistic outcome expectations.
Initial postoperative appearance overestimates final results due to temporary edema (swelling) and the presence of fat cells that will not ultimately survive. During the first 2-4 weeks, you’ll experience gradual volume decrease as swelling resolves and non-viable fat cells are reabsorbed by your body. This early volume reduction represents a normal part of the healing process rather than a complication.
Long-term volume retention typically ranges from 50-70% of the initially transferred fat. Multiple factors influence this retention rate, including harvesting and processing techniques, injection methodology, recipient site vascularity, and individual patient characteristics. Modern techniques have substantially improved these rates compared to earlier approaches that often saw only 30-40% permanent retention.
The timing of stabilized results occurs at approximately 3-4 months post-procedure, when all non-viable fat has been reabsorbed and surviving cells have established permanent blood supply. This represents the true baseline from which long-term results should be assessed. Subsequent volume fluctuations typically correlate with overall weight changes rather than additional loss of transferred fat.
For patients seeking specific size increases, I often plan for staged procedures with 3-6 month intervals between sessions. This sequential approach allows precise, controlled enhancement while ensuring optimal conditions for fat survival in each stage. Most patients achieve their desired results within 1-3 sessions, depending on initial breast size and enhancement goals.
Research demonstrates that fat cells surviving beyond the 3-4 month mark typically remain permanent, behaving identically to native fat cells in the breast. These transferred adipocytes respond to hormonal influences and weight fluctuations just like natural breast tissue, contributing to the completely natural integration of results.
Body type considerations
Your body type significantly influences both candidacy and expected outcomes for fat transfer breast augmentation. Understanding these relationships helps establish realistic expectations and determine whether this approach aligns with your aesthetic goals.
For patients with an ectomorph body type (naturally thin with minimal body fat), fat transfer augmentation may present significant limitations. Your limited donor fat may restrict the total volume available for transfer, potentially making meaningful enhancement challenging. In extremely lean patients with minimal subcutaneous fat, alternative augmentation approaches often prove more appropriate unless only very modest enhancement is desired.
If you have a mesomorph body type (athletic with moderate natural curves), fat transfer often provides excellent options. Your typically well-defined areas of localized fat deposits offer good donor sites while maintaining sufficient fat for harvest without creating contour depressions. Athletic patients particularly appreciate the natural feel and movement of fat transfer results during physical activity, as the enhancement integrates completely with existing tissues without the potential movement restrictions sometimes associated with implants.
Endomorph body types (naturally curvier with more adipose tissue) generally achieve excellent results with fat transfer augmentation. Your abundant donor fat allows maximal volume transfer while creating beneficial contour improvements at liposuction sites. The primary consideration involves proper distribution of the transferred fat to create natural shape enhancement rather than simply adding size. For larger-framed patients seeking substantial enhancement, the combined aesthetic improvement of both liposuction contouring and breast enhancement often proves particularly satisfying.
Existing breast tissue characteristics significantly impact fat transfer outcomes beyond just body type. Patients with dense, well-vascularized breast tissue typically demonstrate superior fat retention rates compared to those with primarily fatty breast composition. The enhanced blood supply in glandular-dominant breasts supports better fat cell survival and integration.
Skin elasticity represents another critical factor in determining appropriate candidacy. If you have good skin tone and elasticity, the transferred fat creates enhanced projection and upper pole fullness. Conversely, if you have significant skin laxity or ptosis (sagging), fat transfer alone may accentuate these issues without addressing the skin envelope concerns. In such cases, combining fat transfer with mastopexy (breast lift) procedures often provides optimal results.
Prior breast surgery impacts fat transfer approach and outcomes. If you’ve previously undergone implant removal, fat transfer can effectively address the tissue thinning or contour irregularities sometimes seen after explantation. However, the altered breast architecture and potential scar tissue require specialized injection techniques to ensure proper fat distribution and integration.
Desired outcome factors
Regarding breast size increase, fat transfer provides modest enhancement rather than dramatic enlargement. You can typically expect a maximum increase of one-half to one cup size per session, with the potential for additional enhancement through staged procedures. Unlike implant-based augmentation where specific volume can be selected, fat transfer outcomes depend on your tissue acceptance and retention rates, introducing some unpredictability. Patients seeking substantial size increases may require multiple sessions or might be better served by implant-based techniques.
For breast shape enhancement, fat transfer excels at creating subtle, natural contours. The technique allows precise targeting of specific areas like the upper pole, medial fullness, or cleavage enhancement. This selective augmentation capability proves particularly valuable for addressing mild asymmetries or contour irregularities. The enhancement integrates seamlessly with your existing breast tissue, avoiding the distinct edges or boundaries sometimes visible with implants in thin patients.
Regarding breast feel, fat transfer provides unparalleled naturalness, as the enhancement consists entirely of your own living tissue. The transferred fat becomes indistinguishable from native breast tissue, maintaining identical softness and consistency. This aspect particularly benefits patients who prioritize natural tactile qualities or those who experienced unnatural firmness with previous implants.
For breast movement, fat-enhanced breasts demonstrate completely natural dynamic properties. The transferred fat moves in synchrony with your existing breast tissue during activity or position changes. This creates fluid, natural-appearing animation without the occasional movement restrictions noted with submuscular implants or the unified movement sometimes seen with subglandular devices.
Fat transfer particularly excels at correcting specific breast concerns beyond simple enlargement. If you have mild asymmetry, the technique allows precise volumetric adjustment between breasts. For tuberous breasts with constricted lower poles, strategic fat placement can expand the constricted tissues while enhancing overall volume. Patients with contour irregularities from previous surgeries, trauma, or congenital conditions often achieve excellent correction through targeted fat grafting.
The dual-benefit nature of fat transfer represents a significant consideration for many patients. The procedure not only enhances breast size but simultaneously improves body contours through strategic liposuction. This combined approach often creates overall aesthetic improvement exceeding what either procedure alone would achieve. For patients with localized fat deposits resistant to diet and exercise, this aspect provides substantial additional value.
Side Effects
All breast enhancement procedures carry potential side effects, and fat transfer augmentation presents specific considerations you should thoroughly understand before proceeding.
Contour irregularities represent the most common aesthetic concern, occurring in approximately 7-10% of patients to some degree. These irregularities may manifest as subtle lumpiness, visible or palpable nodules, or areas of asymmetric volume distribution. Most resolve spontaneously within 3-6 months as the transferred fat integrates and stabilizes. Persistent irregularities can typically be addressed through focused massage or, if necessary, additional fat grafting to smooth affected areas.
Oil cysts (also called fat necrosis) develop in approximately 2-5% of patients when areas of transferred fat fail to establish adequate blood supply but become encapsulated rather than reabsorbed. These benign cysts appear as firm, sometimes tender nodules that may be visible on imaging studies. Most remain small and asymptomatic, requiring no intervention. Larger or symptomatic cysts may need drainage or surgical removal, though this proves relatively uncommon.
Calcifications from fat transfer can develop over time as a normal response to fat cell death during the integration process. These microscopic calcium deposits appear differently on mammography than the calcifications associated with breast cancer, typically demonstrating characteristic patterns radiologists can identify as fat necrosis-related. However, these changes occasionally necessitate additional imaging or rarely biopsy to definitively distinguish them from suspicious findings.
Uneven absorption of transferred fat occurs in some degree in most patients, as natural variations in local blood supply and tissue characteristics influence fat survival rates. When significant, this can create visible asymmetry or irregularity requiring additional treatment. I minimize this risk through meticulous micro-droplet injection technique and avoiding excessive volume transfer in any single area.
Donor site concerns include contour irregularities, temporary numbness, and occasionally prolonged swelling. I minimize these through proper patient selection, even distribution of liposuction, and avoiding excessive removal from any single location. Most donor site issues resolve within 3-6 months as tissues fully heal and adapt to the new contours.
Unlike implant-based augmentation, fat transfer eliminates concerns about implant rupture, capsular contracture, or long-term implant replacement. However, the procedure introduces different considerations, including the unpredictability of exact volume retention and the need for adequate donor fat. Additionally, significant weight fluctuations after the procedure may alter results as transferred fat responds to overall body composition changes.
Interference with mammography and breast cancer detection represents an important consideration with any breast procedure. Current evidence indicates that radiologists experienced with post-fat-transfer appearances can accurately distinguish normal post-procedural changes from suspicious findings. I recommend establishing baseline imaging before surgery when appropriate and informing all future imaging facilities about your fat transfer history to facilitate accurate interpretation.
General recovery timeline
- Day 1: Immediate post-operative period characterized by moderate discomfort at both donor and recipient sites. Compression garments in place over liposuctioned areas. Breast support garment without compression recommended. Limited arm movement advisable. Assistance needed for daily activities. Some drainage from liposuction access points normal.
- Days 2-3: Peak swelling occurs at both donor and recipient sites. Bruising typically becomes more apparent. Donor sites often more uncomfortable than the breasts themselves. Limited to light walking within home. Upper body movements restricted to prevent strain on transferred fat. Initial post-operative appointment typically scheduled. Transition to oral pain medication as discomfort decreases.
- Days 4-7: Gradual improvement in discomfort levels. Initial substantial swelling begins subsiding at donor sites while breast swelling may persist. Permitted to shower according to surgeon’s protocol. Continue wearing donor site compression garments continuously. Breast support without compression continues. Limited to household activities with no strenuous movement or exercise. Driving typically restricted while taking prescription pain medication.
- Week 2: Significant reduction in discomfort for most patients. Donor site swelling noticeably decreased but still present. Breast appearance remains larger than final result due to residual swelling. Most patients return to desk-based work or light duties. Continuation of prescribed compression garments for donor areas. Lifting restriction of 5-10 pounds remains in effect. May notice early volume changes in breasts as initial swelling resolves.
- Weeks 3-4: Continued improvement in donor site appearance as swelling diminishes. May begin noticing reduced breast volume as both swelling resolves and non-viable fat begins reabsorption process. Return to light cardio exercise (walking, stationary cycling) permitted. Upper body movements gradually increasing but avoiding chest-specific exercises or activities causing breast bouncing. Compression at donor sites typically continued but may be reduced to partial-day wear.
- Weeks 4-6: Near-complete resolution of discomfort for most patients. Donor sites approaching final contour but may have persistent firmness or swelling. Permission to resume most normal activities except high-impact exercises. Sleeping position restrictions typically lifted. Breast appearance continuing to evolve as fat integration progresses. Volume stabilization beginning but still changing.
- Weeks 6-8: Cleared to gradually resume full exercise regimen starting at reduced intensity. Donor site contours continuing to refine with diminishing firmness. Breast volume continuing gradual reduction toward final stable result. Most external healing complete at liposuction access points with scars still immature and pink/red in appearance.
- Months 3-4: Complete resolution of swelling at both donor and recipient sites. Breast volume stabilized at permanent level, representing true “final result” from the procedure. All normal activities and exercises resumed without restriction. Potential planning for additional sessions if desired enhancement not achieved with initial procedure.
- 1 Year: Complete tissue integration and stabilization. Any residual donor site irregularities unlikely to improve further without intervention. Long-term outcomes established and maintained. Annual follow-up recommended for ongoing monitoring.




